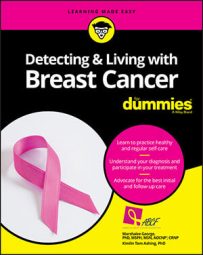
Lumpectomy or partial mastectomy (breast-conserving surgery)
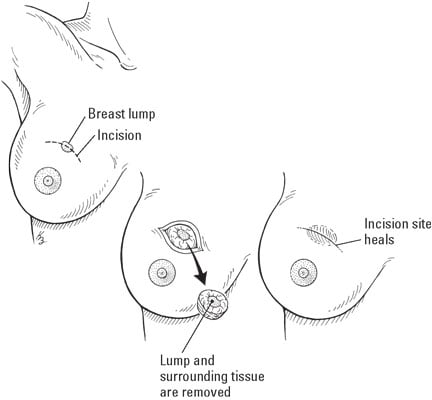
Illustration by Kathryn Born
In a lumpectomy, the lump is removed from the breast as well as a small surrounding area of normal tissue. That is, the entire breast is not removed. Lumpectomy is normally followed by several weeks of radiation therapy.
Mastectomy (total or simple)
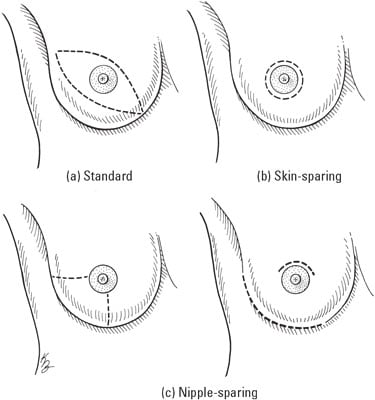
Illustration by Kathryn Born
This is probably what most people think of when they think of breast cancer surgery — removal of the entire breast. When the breast is removed, it is called a total or simple mastectomy. The figure illustrates a few of the possible techniques, each of which has positive and negative aspects.
Modified radical mastectomy
© 2012 Terese Winslow LLC. U.S. Govt. has certain rights
Modified radical mastectomy is when the breast and lymph nodes under the arm are removed. If there are obvious signs or confirmed pathology (from biopsied lymph nodes under the armpit) that the cancer has spread to your lymph nodes, then a modified radical mastectomy can be performed.
Axillary lymph node dissection
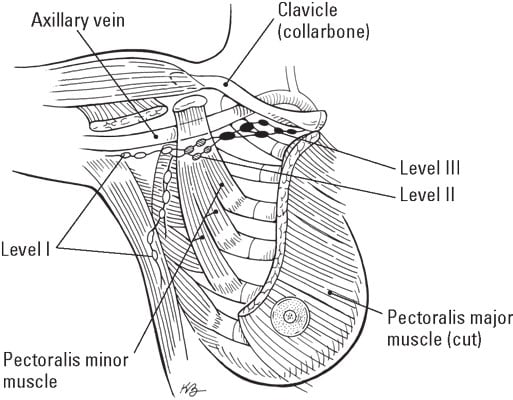
Illustration by Kathryn Born
This type of surgery involves opening the armpit (axilla or axillary) to examine or remove lymph nodes — small glands, part of the lymphatic system, that filter fluid from cells.
Talk to your doctor more about this to determine the best treatment for you.
Axillary lymph nodes have three levels, shown in the figure:
- Level I is the bottom level and located at the lower edge of the pectoralis minor muscle.
- Level II is located underneath the pectoralis minor muscle.
- Level III is located above the pectoralis minor muscle.
Sentinel lymph node biopsy
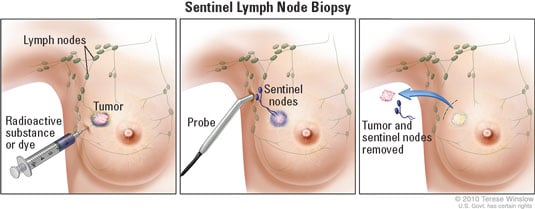
© 2012 Terese Winslow LLC. U.S. Govt. has certain rights
Axillary lymph node dissection may be offered when the cancer has spread to your lymph nodes. However, recent studies have shown benefits of radiation of the lymph nodes instead of axillary dissection for select patients with minimal spread or micro metastasis (microscopic cancer cells) to the axillary lymph nodes and with T1 and T2 tumors (5 cm or less):
- Axillary lymph node dissection: This usually involves the removal of lymph nodes in levels I and II, which can amount to approximately 5–30 lymph nodes. This procedure may be done at the same time with a mastectomy for women who have invasive breast cancer. It also can be done at the same time or after a lumpectomy. The total number of lymph nodes involved (showing evidence of cancer) is more important than the extent of cancer in any one node.
- Prophylactic mastectomy: When a person chooses to remove one or both breasts pre-cancer, because of familial or genetic risk factors, or because of the possibility of re-occurrence of cancer.
- Sentinel lymph node biopsy: The surgeon injects a blue dye and/or a radioactive dye below the nipple area several hours prior to surgery. The highest sensitivity for finding the sentinel node (the first draining lymph node of the breast) is when both dyes are used during the sentinel lymph node biopsy. During surgery the surgeon removes the tumor and is able to find a lymph node that has picked up the dye. The first lymph node to pick up the dye is called a sentinel lymph node. The dye will follow the same path that a tumor cell that breaks off from the main tumor would travel on its way to the lymph node. The dye creates a “trail of bread crumbs” for the surgeon to find the lymph nodes most likely to have tumor cells (that is, lymph node metastasis).