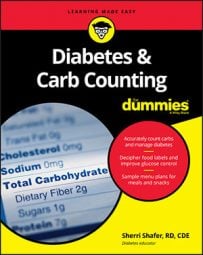
Rapid-acting insulin works its hardest (peaks) about an hour after being injected and finishes working in about four hours. In the figure, the dotted line represents the onset, peak, and duration of rapid-acting insulin. The shaded curve represents the blood-glucose levels rising and resolving after eating. As illustrated, the insulin action and the digestion and absorption of glucose from the meal line up nicely.
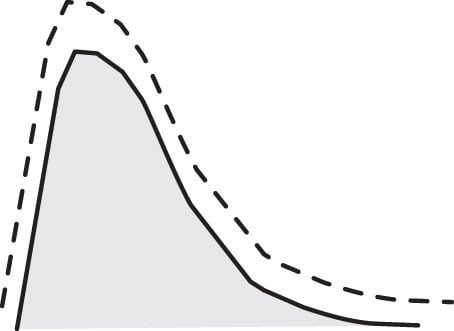
Recall that fatty meals digest slower. The following figure illustrates what may happen when rapid-acting insulin is taken before a meal that has a significant amount of fat. Again, the dotted line represents the timing of the insulin and the shaded curve represents the blood-glucose levels resulting from a high-fat meal.
It may be a meal composed of fried foods, large portions of fatty meat, a cheesy meal, or a meal with a lot of added fats: butter, mayo, sour cream, salad dressing, or guacamole. The rapid-acting insulin works at its normal rate, but the fatty meal digests slower than a normal meal. Consequently, the insulin may peak before the meal digests, which could cause hypoglycemia during the meal. Later, when the food finally digests, the insulin has passed its peak and doesn't have enough strength to lower the blood glucose, so glucose levels remain elevated. Such a situation can lead to high blood-glucose levels at bedtime after eating a high-fat dinner.
One solution may be to take the insulin midway through the meal or toward the end of the meal. Giving a fatty meal a head start can improve the way the insulin and the blood-glucose timings align.
Discuss adjustments to injection timing with your healthcare provider prior to making changes to your regimen.