You should be familiar with the nuts and bolts of myocardial infarction (MI for short) for your Physician Assistant Exams. A person is said to be having an MI if there’s a positive enzyme leak in the blood and accompanying ECG changes. The clinical presentation may not always be reliable. For example, you may miss an MI in a person with diabetes and bad neuropathy.
You should also be aware of some of the labs used in evaluating an MI. Here are a couple of points:
The troponin I rises within the first few hours of an MI and can stay elevated for at least a week, if not more.
The creatine phosphokinase (CPK) and the CK-MB fraction especially start rising in the first few hours but peak in around a day, only to return to baseline in about 2 to 3 days.
The thrombolysis in myocardial infarction (TIMI) score is a great scoring system that any clinician can use during the history and physical. This scoring system is based on cardiac risk factors as well as known coronary artery disease. You can use the TIMI score to risk-stratify patients being admitted to the hospital.
There are two types of myocardial infarctions, depending on how much of the myocardium is affected. NSTEMI stands for non-ST-elevation myocardial infarction. This MI doesn’t involve the entire myocardium. It’s not a transmural MI. A diagnosis of NSTEMI is made by positive cardiac enzymes, and you’ll likely see ST depression or T-wave inversion on the ECG, indicating that ischemia is going on.
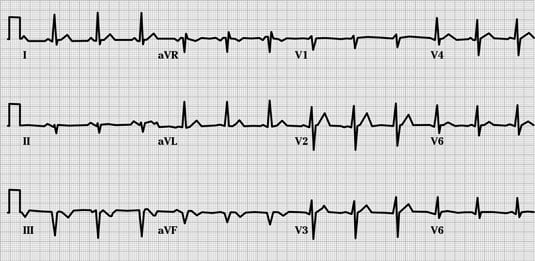
STEMI stands for ST-elevation myocardial infarction. This is the biggie, reflecting an infarct that affects the whole wall of the myocardium. Classic ECG patterns include hyperacute ST segment elevation with (later on) the formation of a Q wave when the infarct is complete. Here are some specific patterns to be aware of concerning STEMI as seen on the ECG:
Anterior wall myocardial infarction: This causes ST elevation in leads V1 through V3, and it can also affect V4. The coronary artery affected is the left anterior descending (LAD), which supplies the left ventricle. Common clinical presentations of an acute anterior wall myocardial infarction can include acute pulmonary edema and cardiogenic shock.
Inferior wall myocardial infarction: This MI causes an ST elevation in leads II, III, and aVF on an ECG. Someone with an inferior wall MI can present with nausea, vomiting, and GI upset. The inferior wall sits near the vagus nerve; consequently, an MI in this area can mimic GI symptoms via vagal nerve stimulation. The artery affected by an inferior wall MI is the right coronary artery.
Here are some other key points concerning an inferior wall MI:
If you see a test question in which a person with an inferior wall MI presents with hypotension, there may be extension of the inferior wall MI to affect the right ventricle.
In another scenario, a person with an inferior wall MI is given nitroglycerin to help with the chest pain and all of a sudden experiences a drop in blood pressure. There’s extension to involve the right ventricle and hypokinesis of that right ventricle. The treatment is fluids, fluids, fluids, with isotonic saline to increase preload.
Another complication of an inferior wall MI is a ventricular septal defect.
Lateral wall MI: There’s a high lateral wall MI and a low lateral wall MI. You see ST segment elevation in leads I and aVL for an MI in the high lateral wall, and ST segment elevation in leads V5 and V6 for an MI in the low lateral wall. A STEMI of the high lateral wall can affect the circumflex artery. There are usually no significant hemodynamic complications.
Posterior wall MI: This MI can be a tricky one to determine. The clinical presentation can be similar to an inferior wall MI (that is, GI symptoms can predominate). On an ECG, you see ST depression in the anterior leads (V1 and V2 big time). You need to use the mirror trick: Flip the ECG over to see the ST elevation.
Just because someone comes into the hospital on warfarin (Coumadin) doesn’t mean that he or she can’t have an MI. Warfarin isn’t an antiplatelet drug; it works on the extrinsic clotting pathway. Warfarin doesn’t inhibit platelet aggregation/clumping. That’s why aspirin and clopidrogel (Plavix) are used in treating acute coronary syndrome.
You need to be aware of several important points concerning ECG interpretation of a STEMI:
During an acute MI, there’s initially T wave elevation that converts to hyperacute ST segment elevation. You often see ST segment elevation in two contiguous leads in the setting of a STEMI.
Within a few hours, you can begin to see negative T waves or T wave inversion as the MI evolves. The T wave inversion can persist for months after the MI.
A Q wave can take hours to days to develop (depending on the MI) and means that the damage done to that particular area is irreversible. Q waves are in the inferior leads, meaning that in a recently completed MI, either the MI has run its course or it’s an old inferior wall MI.
 Credit: ©1997–2010 Intermountain Healthcare. All rights reserved.
Credit: ©1997–2010 Intermountain Healthcare. All rights reserved.