 © Leremy / Shutterstock.com
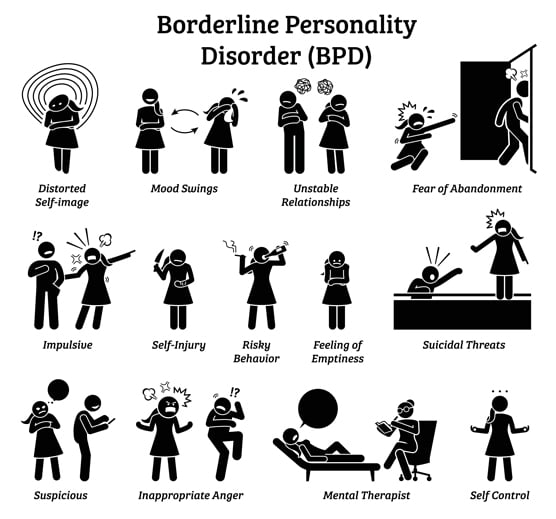
© Leremy / Shutterstock.comThe symptoms of borderline personality disorder
Diagnosing borderline personality disorder (BPD) is complex, even trained mental health professionals may have difficulty with the diagnosis because the symptoms of BPD can vary dramatically between people. A range of BPD symptoms exist and are grouped into nine categories. To be diagnosed with BPD you must frequently exhibit at least five of these nine symptoms:
-
Intense worries about abandonment and strong efforts to avoid it
-
Unpredictable, rocky relationships
-
Uncertainty about self-identity
-
Reckless, risky behaviors
-
Self-harming behaviors
-
Highly volatile emotions
-
Profound feelings of hollowness or emptiness
-
Easily provoked rage
-
Short-term flights from reality
Important Information about borderline personality disorder
Don’t despair if you’re diagnosed with borderline personality disorder. Seeking help and finding the right treatment can be effective. Keep these things in mind:
-
Remember that BPD doesn’t define who you are. Try to view your symptoms as your BPD at work — not you.
-
If you have BPD, realize that you have lots of company. Many millions of people have the same problem.
-
Understand that treatment for BPD works, but it does take time and effort.
-
Don’t rely on medications alone for help with your BPD problems — they won’t suffice.
-
Know that other problems, such as anxiety, depression, and substance abuse, often accompany BPD. These problems may require specific treatment in addition to the treatment you receive for BPD.
-
Try to realize that your therapist is on your side. Your fears of abandonment may cause you to push your therapist away — try to resist this tendency.
Tips for friends and family of someone with borderline personality disorder
It can be difficult to deal with a friend or loved one who has borderline personality disorder (BPD). Use these tips to handle tough times and help maintain a safe environment:
-
Read as much as you can about BPD — knowing about the disorder helps you deal with it.
-
If you live with someone who has BPD, join a support group or consider therapy for yourself to help you deal with the issues you face.
-
Understand that BPD behaviors aren’t about you. Try to depersonalize what’s happening.
-
Even if you understand BPD behaviors, you need to know your own limits and stick by them — don’t ever allow yourself to be abused.
-
Understand your loved one’s hot buttons and try not to push them — yet know that you won’t always succeed.
-
Realize that sometimes the only thing you can do is leave the relationship when your loved one repeatedly runs over your limits or when your loved one refuses treatment.
Useful tips for people with borderline personality disorder
People with borderline personality disorder (BPD) usually exhibit behaviors, feelings and thoughts in drastic forms. Try these things to help you manage impulsive behavior and extreme thinking when dealing with BPD:
Slowing down impulsiveness:
-
When a question or comment upsets you, wait at least five seconds before responding and repeat “calm down” in your mind several times first.
-
When you feel a strong impulse, remind yourself that taking action at those times usually results in bad outcomes.
-
Discuss with your therapist any new, big plans you might have for your life before taking action.
-
Practice breathing exercises often.
Cooling down extreme thoughts:
-
When you have an extreme or “hot” thought, ask yourself how a friend may look at the same issue differently.
-
When your thoughts are strong and extreme, ask yourself how you may view the triggering event six months down the road and notice the difference.
-
Remember that extreme words and phrases such as always, never, can’t stand it, awful, and horrible are almost always inaccurate. Try to find the shades of gray.