Oogenesis (the egg-producing process), which includes the ovarian and menstrual cycles, begins very early in the life of a human female, when she’s still a developing fetus! In fact, a human female is born with all the eggs she’ll ever have.
However, the eggs aren’t quite finished, because cell division pauses early in the first half of meiosis. These eggs lie dormant from birth until puberty, at which time the monthly cycle of a woman’s hormones restarts the development of eggs — usually one per month.
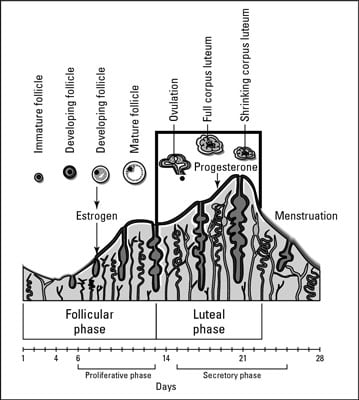
Thus, two reproductive cycles in the female regulate human sexual reproduction (see the figure that follows in this article):
The monthly ovarian cycle regulates development of the egg in the ovary. The ovarian cycle includes the development of the follicle, the secretion of hormones by the follicle, ovulation, and the formation of the corpus luteum. It occurs in the ovary, takes about 28 days, and is controlled by the hormones gonadotropin-releasing hormone (GnRH), follicle-stimulating hormone (FSH), luteinizing hormone (LH), and estrogen.
The monthly menstrual cycle refers to the periodic series of changes that prepare the female body for the implantation of an embryo. The menstrual cycle includes the thickening of the endometrium to prepare for possible implantation of an embryo and the shedding of the endometrium if no embryo is implanted. It occurs in the uterus, takes about 28 days, and is controlled by the levels of the hormones progesterone and estrogen.
Ultimately, the brain controls the ovarian cycle by releasing hormones from two glands at its center. The hypothalamus monitors the levels of estrogen and progesterone in the blood. When the levels decline, the hypothalamus secretes GnRH, which goes straight to the pituitary gland and stimulates part of the pituitary to secrete FSH and LH.
The hormones from the brain control the levels of estrogen and progesterone released by the female reproductive system, leading to the events of the ovarian cycle:
A follicle starts to grow and begins producing the hormone estrogen.
About midway through the ovarian cycle, estrogen reaches a critical level, causing the hypothalamus to release more GnRH.
The GnRH triggers the pituitary gland to release a burst of LH and FSH.
The spike in LH triggers the completion of meiosis so that the egg finishes its development.
LH stimulates enzymes that break open the follicle, causing ovulation, the release of the egg from the follicle.
LH also triggers the remaining follicle cells to develop into a mass of cells called the corpus luteum, which secretes estrogen and progesterone for the rest of the ovarian cycle (about two more weeks).
Estrogen and progesterone prepare the body for a possible pregnancy by spurring the tissues lining the uterus to develop thicker blood vessels.
These hormones send negative feedback to the hypothalamus and pituitary, reducing the production of FSH and LH and thus preventing the development of more follicles.
The corpus luteum breaks down after about two weeks, and if implantation of a fertilized egg doesn’t occur, the levels of estrogen and progesterone fall. The entire ovarian cycle begins again.
 Credit: From LifeART®, Super Anatomy 1, © 2002, Lippincott Williams & Wilkins
Credit: From LifeART®, Super Anatomy 1, © 2002, Lippincott Williams & Wilkins
The progesterone and estrogen from the ovarian cycle also control the menstrual cycle:
If implantation doesn’t occur and the levels of estrogen and progesterone fall, the endometrium sloughs off, and menstrual bleeding begins.
As the levels of estrogen begin to rise, the endometrium thickens. This thickening continues as progesterone levels increase.
The first day of menstrual bleeding marks the first day of the menstrual cycle.
If a fertilized egg does implant in the uterus’s lining, the developing embryo releases a hormone called human chorionic gonadotropin (hCG). The presence of hCG maintains the corpus luteum, thus keeping up production of the estrogen and progesterone necessary to maintain the endometrium.
After the placenta (a blood-filled, nutrient-rich, temporary organ) has formed, the embryo gets its nutrients and blood supply through the umbilical cord connecting the embryo to the placenta, which is connected to the mother’s blood supply. Therefore, the embryo’s production of hCG declines after the placenta is up and running.
Use the terms that follow to identify the role of each hormone. Some questions may have more than one correct answer.
a. FSH
b. LH
c. hCG
d. GnRH
e. Estrogen
f. Progesterone
Falling levels of this trigger the start of menstruation.
It stimulates the pituitary to make FSH and LH.
It triggers growth of the follicle.
It causes rupture of the follicle and ovulation.
Rising levels of this stimulate development of the endometrium.
It prevents breakdown of the corpus luteum.
The following are the answers to the practice questions.
The answer is e. Estrogen and f. Progesterone.
The answer is d. GnRH.
The answer is a. FSH and b. LH.
The answer is b. LH.
The answer is e. Estrogen and f. Progesterone.
The answer is c. hCG.